Restful Nap FAQ – CPAP, Oral Appliances, and Sleep Apnea
Most questions center on treatment choices, so this FAQ helps you weigh options: CPAP is the most effective therapy for moderate‑to‑severe sleep apnea, while oral appliances can improve symptoms in mild‑to‑moderate cases; you should also know that untreated sleep apnea raises your risk of heart disease, stroke, and daytime accidents, and adherence to therapy is key to safer, more restorative sleep.
Key Takeaways:
- CPAP is the most effective treatment for moderate-to-severe obstructive sleep apnea: it uses continuous positive airway pressure to prevent airway collapse, and consistent nightly use plus proper mask fit and follow-up maximize benefits.
- Oral appliances (mandibular advancement devices) are a good alternative for mild-to-moderate OSA or CPAP-intolerant patients: they advance the lower jaw to open the airway, are fitted by a dentist, and may require periodic adjustments and dental monitoring.
- Treatment choice depends on diagnosis and patient factors: confirm OSA severity with a sleep study, consider anatomy, comorbidities, and adherence potential, and combine device therapy with weight management, positional therapy, and regular outcome follow-up.
Understanding Sleep Apnea
Repeated pauses in breathing fragment your sleep and raise your risk of hypertension, metabolic dysfunction, and daytime accidents. You may have loud snoring, gasping arousals, or persistent fatigue; severity is measured by the apnea‑hypopnea index (AHI) with thresholds: mild 5-15, moderate 15-30, severe >30. Treatments like CPAP and oral appliances reduce symptoms and lower cardiovascular risk, while untreated disease increases stroke and heart‑attack likelihood.
What is Sleep Apnea?
You have sleep apnea when airway obstruction or impaired respiratory drive causes repeated breathing pauses, oxygen drops, and sleep fragmentation; symptoms include snoring, choking, and daytime sleepiness, and diagnosis uses polysomnography or home testing to quantify AHI. Typical AHI cutoffs guide therapy selection and risk stratification. After diagnosis, you and your clinician choose targeted treatment based on type and severity.
- Apnea‑Hypopnea Index (AHI)
- Obstructive sleep apnea (OSA)
- Central sleep apnea (CSA)
- CPAP
- Oral appliance
| Definition | Repeated airflow pauses from airway collapse or reduced drive |
| Common signs | Loud snoring, witnessed apneas, daytime sleepiness |
| Severity (AHI) | Mild 5-15, Moderate 15-30, Severe >30 events/hour |
| Risk factors | Obesity, male sex, age, alcohol, sedatives |
| Health impact | Increased risk of HTN, stroke, MI, and motor-vehicle crashes |
Types of Sleep Apnea
You’ll encounter three main types: Obstructive (upper‑airway collapse), Central (reduced respiratory drive), and Complex (mixed features). OSA makes up the bulk of cases and closely tracks with obesity and airway anatomy; CSA is less common and often linked to heart failure or opioid use. Treatment strategies differ-CPAP and oral appliances for OSA, targeted therapy for CSA-so precise classification matters. After identifying the type, therapy is individualized to your physiology and risk profile.
- Obstructive sleep apnea (OSA)
- Central sleep apnea (CSA)
- Complex/mixed apnea
- CPAP
- Adaptive servoventilation (ASV)
| Type | Obstructive, Central, or Complex (mixed) |
| Mechanism | Upper‑airway collapse vs. impaired drive vs. both |
| Prevalence | OSA most common; CSA less than 10-15% in many series |
| Common causes | Obesity/anatomy (OSA); heart failure, stroke, opioids (CSA) |
| Typical therapy | CPAP, oral appliance, positional therapy, ASV or oxygen as indicated |
In practical terms, OSA often worsens in REM and supine position and responds well to positional therapy or mandibular advancement for mild‑moderate disease; oral appliances can reduce AHI by roughly half in selected patients, while CPAP normalizes airflow but requires adherence monitoring (~>4 hours/night target). CSA frequency rises with heart failure and opioid exposure and may need ASV or supplemental oxygen in specific contexts. After you track symptoms and device adherence, repeat testing guides next steps.
- Positional therapy
- Mandibular advancement device
- CPAP adherence
- ASV
- Follow‑up polysomnography
| Triggering factors | Supine sleep, REM, alcohol, sedatives |
| Therapy impact | Oral appliances reduce AHI ~30-50% in mild-moderate cases |
| Adherence threshold | Common benchmark: >4 hours/night on ≥70% of nights |
| CSA associations | Heart failure, atrial fibrillation, opioid therapy |
| Follow‑up | Symptom tracking, device downloads, repeat sleep testing as needed |
Importance of Restful Naps
If you have sleep apnea, well-timed naps can reduce daytime sleepiness and improve cognitive performance; they do not replace CPAP or oral appliances. Short naps lower crash risk and can complement treatment when you maintain your nightly therapy and timing. For more on oral appliance guidance, see Q&A About Oral Appliances for Sleep Apnea – Northgate Dental.
Benefits of Napping
You can use a 10-20 minute nap to quickly restore alertness, reaction time, and mood; 30-60 minute naps support memory consolidation but may cause brief grogginess. Clinical data show brief naps improve performance for up to 2-3 hours and reduce driving-related impairment, making naps an effective short-term strategy when nighttime sleep is fragmented by apnea.
Ideal Nap Duration
For immediate alertness aim for 10-20 minutes; choose a 90-minute nap to complete one sleep cycle and minimize inertia; 30-60 minutes helps procedural memory but can leave you drowsy afterward.
Timing matters: avoid naps after 3 PM to prevent delayed sleep onset at night. If you use CPAP or an oral appliance, nap with your therapy when possible to preserve airway stability and oxygenation. Track nap length and daytime sleepiness-if you still feel excessively sleepy despite short, well-timed naps and therapy, consult your provider because persistent sleepiness may indicate residual apnea, suboptimal device settings, or another sleep disorder.
CPAP Therapy
For many people, CPAP provides the most reliable way to stop airway collapse and restore sleep continuity. When you use prescribed pressure nightly, CPAP can reduce apneas by up to 90%, markedly improving daytime alertness and lowering cardiovascular strain seen in moderate-to-severe OSA. Aim for consistent use-most benefits appear once you use it ≥4 hours per night on the majority of nights.
How CPAP Works
CPAP delivers a steady stream of air that splints your upper airway, preventing collapse during sleep; pressures typically range from 4-20 cm H2O. Auto-adjusting devices (APAP) change pressure breath-by-breath to address events, and heated humidification reduces congestion and nasal dryness. You’ll choose between nasal, nasal-pillow, or full-face masks based on your breathing pattern and leak control.
Adjusting to CPAP
Start gradually by wearing your mask during short naps and at bedtime, use the ramp feature to ease into prescribed pressure, and work toward that ≥4 hours/night benchmark; many patients notice meaningful improvement within two weeks. Schedule a follow-up or telecheck within 2-4 weeks to fine-tune pressure and mask fit.
If you struggle, address leaks by trying different mask types, add heated humidification for dryness, use a chin strap for mouth leak, or enable pressure-relief modes (C-Flex/EPR). Practice desensitization-wear the mask while awake, take short naps, and use relaxation techniques. Replace the mask every 3 months, tubing every 3-6 months, and filters monthly; contact your clinician if you still have excessive daytime sleepiness, persistent gasping, or new morning headaches.
Oral Appliances
What are Oral Appliances?
You wear a mandibular advancement device (MAD) that gently pulls your lower jaw forward to enlarge the airway and reduce collapse during sleep. Custom, dentist‑fitted devices are titratable and generally work better than over‑the‑counter boil‑and‑bite models for comfort and results. Typical advancement ranges 4-8 mm and you can use them nightly or for naps. Prescription, custom appliances are more effective and better tolerated, and coordinated care with a sleep physician improves outcomes.
Effectiveness and Fit
You can expect about a 50% average reduction in AHI with a well‑fitted MAD; complete normalization occurs in roughly 30-40% of patients with mild‑to‑moderate OSA. Higher nightly use compared with CPAP often improves real‑world effectiveness, especially for travel or intolerance to masks. If you have severe OSA, CPAP remains the safer choice. Proper fit requires dental impressions, bite registration, and periodic titration by a sleep‑trained dentist.
You should plan objective follow‑up: a home sleep test or PSG after titration confirms efficacy and guides adjustments, aiming for AHI <5 events/hour when possible. Expect short‑term jaw soreness and, over years, dental occlusal changes in some patients-bite changes have been reported in up to 30% with long‑term use. Insurance often requires documented improvement, so keep records of testing and adjustments.
Combining Treatments
CPAP vs. Oral Appliances
You should weigh effectiveness against tolerability: CPAP typically reduces apnea‑hypopnea index (AHI) by >90% when used nightly and is the standard for severe OSA (AHI >30), while oral appliances average a ~40-60% AHI reduction and succeed in about half of mild-moderate cases. If mask intolerance limits your use, oral appliances often improve nightly adherence, but you’ll trade some efficacy for comfort. Discuss your AHI, sleepiness score, and tolerance to guide the choice.
Personalized Treatment Plans
Your plan should combine objective measures and preferences: AHI, BMI, jaw anatomy, positional dependency, dental health, and comorbidities determine whether CPAP, an oral appliance, positional therapy, weight loss, or surgery best fit. Clinicians commonly recommend CPAP for AHI ≥15 or significant daytime sleepiness, and consider oral appliances for AHI <15 or CPAP intolerance. Shared decision‑making plus measurable goals (AHI target, symptom reduction) guides selection.
For more detail, clinicians often use structured pathways: if you have mild OSA (AHI 5-15) and favorable jaw anatomy, an oral appliance trial with a post‑fitting home sleep test within 4-12 weeks can confirm success; if you present with AHI ≥15 or cardiovascular disease, expect immediate CPAP to be advised with follow‑up at 1-3 months to check adherence and residual AHI. Combining therapies-such as using an oral appliance to lower CPAP pressure, adding positional therapy, or targeting a 5-10% weight loss-can improve outcomes; confirm effectiveness with objective testing and adjust the plan accordingly.

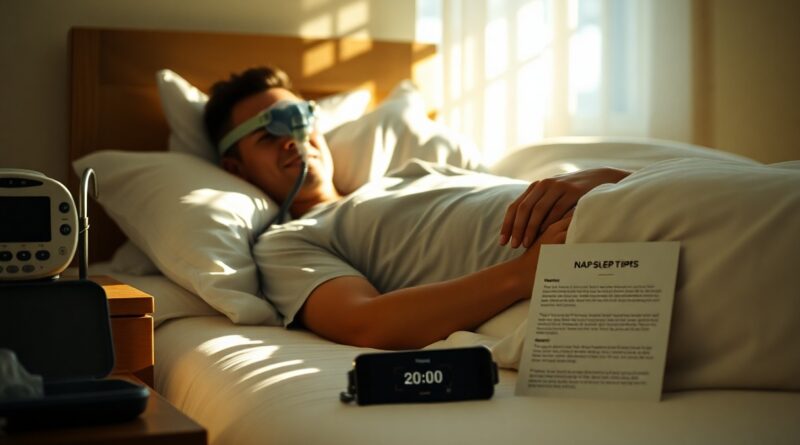
Tips for Optimal Napping
Quick, evidence-based steps to make naps effective:
- Set an alarm for 10-30 minutes to avoid deep-sleep inertia
- Schedule naps between 1-3 PM when circadian dip occurs
- Use your prescribed CPAP or oral appliance during naps if directed
Limit caffeine 4-6 hours beforehand and keep light/noise low. This FAQs About Oral Appliance Treatment for Sleep Apnea explains appliance use during naps.
Creating a Sleep-Friendly Environment
Optimize your nap setting by keeping the room dark, quiet, and cool (60-67°F); use blackout curtains, earplugs or a white-noise device at ~40-50 dB, and remove screens 30-60 minutes before lying down. You should also use a supportive pillow and, if recommended, your oral appliance to help maintain airway patency while you nap.
Best Practices for Restful Naps
Adopt a consistent nap routine: aim for 10-30 minutes to boost alertness without disrupting nighttime sleep, keep naps to the early afternoon, and avoid napping late or longer than 45 minutes to prevent sleep inertia. If you have sleep apnea, coordinate nap timing and device use with your treatment plan.
Short naps of 10-20 minutes reliably improve reaction time and alertness for up to about 3 hours; longer naps (30-45 minutes) can aid memory consolidation but raise the risk of grogginess. If your AHI is elevated or you have uncontrolled OSA (for example, AHI >15), discuss nap strategies with your provider and ensure you use prescribed therapy-CPAP adherence or a fitted oral appliance reduces apnea events during daytime sleep and improves safety and effectiveness.
Summing up
On the whole, you should view CPAP and oral appliances as complementary tools to manage sleep apnea and improve naps; CPAP remains most effective for moderate-severe cases, while custom oral devices can help mild to moderate apnea and CPAP intolerance. Work with your sleep specialist for diagnosis, fitting, and follow‑up to optimize comfort, adherence, and daytime rest.
FAQ
Q: What are the primary differences between CPAP and oral appliance therapy for obstructive sleep apnea?
A: Short answer: CPAP (continuous positive airway pressure) delivers pressurized air to hold the airway open and is the most effective treatment for moderate-to-severe obstructive sleep apnea (OSA); oral appliances (usually mandibular advancement devices, MADs) reposition the lower jaw to enlarge the airway and are most effective for mild-to-moderate OSA or patients who cannot tolerate CPAP. Key differences: 1) Mechanism – CPAP provides pneumatic splinting; MAD mechanically advances the mandible. 2) Effectiveness – CPAP typically reduces AHI more reliably across severity levels; MADs often reduce AHI substantially in mild-to-moderate cases. 3) Adherence and comfort – some patients tolerate MADs better, improving real-world effectiveness despite lower physiologic efficacy. 4) Side effects – CPAP: mask discomfort, nasal congestion, dry mouth; MAD: jaw soreness, bite changes, tooth movement. 5) Practical factors – CPAP needs electricity and regular supply replacement; MAD is portable and dental-based; insurance coverage and upfront costs vary.
Q: How should I use and maintain a CPAP machine or oral appliance to get the best results?
A: Use and maintenance guidelines: CPAP – 1) Use nightly for the entire sleep period; partial-night use reduces benefit. 2) Ensure proper mask fit and pressure settings (work with your sleep clinician for titration or auto-PAP). 3) Clean mask, cushion, and humidifier chamber daily or weekly per manufacturer instructions; replace disposable filters weekly and reusable filters monthly. 4) Typical replacement intervals: mask cushions 1-3 months, mask/frame 3-6 months, tubing 3 months, headgear 6-12 months, device 3-5 years. 5) Monitor use data (hours/night, mask leak, AHI) and follow up with your provider. Oral appliance – 1) Wear nightly as directed and avoid sleeping without it for moderate-to-severe OSA unless advised otherwise. 2) Clean after each use and store properly. 3) Attend dental follow-ups 4-12 weeks after delivery for adjustments, then every 6-12 months to check fit, dental health, and jaw function. 4) Possible long-term effects: occlusal changes and TMJ symptoms; report issues promptly. 5) Verify effectiveness with follow-up sleep testing or device-reported metrics when available.
Q: Who is a good candidate for an oral appliance instead of CPAP, and can therapies be combined?
A: Candidate profile and combination options: Good candidates for an oral appliance are patients with mild-to-moderate OSA, those with lower AHI and lower BMI, or patients who cannot tolerate CPAP despite troubleshooting. Candidates must have adequate dentition and no active periodontal disease or severe temporomandibular joint disorder. Oral appliances are generally not recommended as sole therapy for severe OSA unless monitored closely by a sleep specialist. Combination therapy is used when CPAP pressure needs are high or adherence is poor: using a MAD together with lower-pressure CPAP can improve comfort and adherence and may reduce required pressure; this should be prescribed and monitored by a sleep physician and qualified dentist. In all cases, objective follow-up (repeat sleep testing or device data) is required to confirm that apnea is controlled and to guide adjustments.